Articles/Blogs
DR. ANDREW DEAN
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
“Why should I need mindfulness, as an ED Clinician?”
So the answer is, of course you don’t – if you see no value in it for you.
Mindfulness techniques do not change the system structures that create bed block, patient overcrowding or work-related stress in the ED, but are tools that help us optimise our response to such stress, and to alter our emotional reactivity to events happening around us.
Techniques of mindfulness are like a counter-conditioning for our brain’s default patterns of emotional reaction patterns, to external or internal triggering events and thoughts. We assume that we are always going to react in essentially the same way to stresses, and that our brains are ‘hard-wired’ to react in the same way, every time. In other words, that we
essentially don’t have much control over this, because the way we are is the way we are.
Not so.
ACEM supports Wellness and has a network of Wellness Champions who are all working towards linking ED Clinicians with concepts of self-sustaining and resilient behaviours.
A component of the various elements of Wellness is mindfulness, which from my own and others’ experience can be incorporated into the busy life of a front-line ED Clinician. You might be surprised (I was) at just how many of your colleagues are already on this path, utilising daily mindfulness practice to facilitate their effective clinical work.
So don’t take it from me, but you may want to explore some of the many mindfulness apps, or look at some scientific evidence – a good starting point are the following resources:
Treat: a free mindfulness app from the Alfred Hospital for critical care and emergency department staff. Free app for all IOS or Android devices Smiling Mind
Headspace
College and collegial Wellness resources
ACEM Wellness Week: August 15-21, 2021,
WRaP EM
wrapem.org
And for a look at the science of neuropsychology and how mindfulness works, A/Prof Craig Hassed (Monash Wellbeing) explains the evidence and science for the benefits of mindfulness in these two videos:
https://youtu.be/IsXxvPWd_k4
https://youtu.be/9O7vd2uGO0w
Many professional groups are working mindfulness into their routines for their key personnel, and emergency medicine should not be any different. Burnout, early retirement and mental health problems are all too common in our ED colleagues. This Wellness stuff is clearly very important, and I am convinced that we owe it to ourselves to at least examine what mindfulness is, and perhaps try some of the options available (most of them are completely free).
In the next article I will discuss how our brain reacts to stress, and how mindfulness changes this. And yes, it is all scientifically proven, and yes, it does work.
Take care of yourself and thanks for reading this.
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
“I agree that I am stressed, but I can’t change that”
We all have default ways of reacting to stress and these “built in” patterns are regarded as fixed, or intrinsic, parts of our personality.
“He is just like that; he can’t help it. It is just a pity he is the Director!”.
We react emotionally and physiologically to stressful situations and people around us at work or home, and may be triggered to be annoyed, angry, resentful or to lose our sense of equilibrium and balance. These emotional reactions may be externalised (so called “outbursts”), or kept within while we maintain a calm exterior to the world (I suppose you could call the internalised reaction an “inburst”). Either pattern of reaction can be destructive, and can adversely affect our health as well as our relationships, and the ED “culture” in our workspaces.
Why do we accept so much pain, caused by this emotional reactivity?
These reaction patterns to stress are commonly regarded as being “hard wired”, a part of our personalities, or an inevitable consequence of our life experiences. We repeat these often painful, recurring patterns of reactions to external events, and this can be incredibly exhausting and can also contribute to feelings of “burn-out”.
Mindfulness research tells us that none of us are as “hard wired” as we may think, and that our default reaction patterns can be changed with even relatively brief practice of mindfulness techniques. Setting aside a few minutes each day starts this process.
It could be just by catching ourselves at the start of a familiar irritable feeling, and reminding ourselves that there is another way to see the situation that seems to be triggering us. Taking a few slow breaths, and moving briefly away from other people if we can, creates a mental space for our mind to reset.
A bit like the methods we use in an ED resuscitation, when we recap, invite group inputs, and summarise how the patient is responding to our care. These strategies are healthy.
Starting your day with a few moments of mindfulness practice – keep it really simple, do the three slow consecutive breaths exercise, and envisaging your day going really well – will give you a new way of reacting to stress. Or rather, a strategy for reacting less to stress than you otherwise might have previously.
Keeping a discipline like this, even if only for a few conscious slow breaths, starts an internal process of change. “Brain training” if you like. It works for dogs, so why not brains?
“But I still don’t see the point of all of this..”
And I would completely agree with you that it is not for everyone. But with really diverse and unlikely groups – including primary school kids (seemingly everywhere, these days!), prisoners, US Air Force pilots and ex-criminal shipyard workers in Alaska – incorporating mindfulness into their daily workplace routines, there has to be something to it that is worthy of our consideration. Why would they do it otherwise?
“So, does it actually help you?”
I know that my own various roles in the ED and Hospital environment are dramatically enhanced by having the backdrop of daily mindfulness routines. Hands down, no argument. Less stress, less conflict, less defensiveness, better health. I could simply not do it all, without mindfulness. Period.
For me it is the beginning of the day, but particularly the end of the day when the world gets quiet. Funny thing is, within the day, when we assume we will have no spaces for this stuff, there actually are many opportunities for brief mindful moments – waiting for coffee, walking to CT to get a verbal report, typing up notes – when we can recalibrate and do a mental “check in” on ourselves. A quick “maintenance check” on the hard drive perhaps…
Next time let’s get into specifics and away from the general discussion about benefits. Because unless you actually try it, it is just theory…
Take care of yourself and thanks for reading this.
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
“Why would I benefit from mindfulness?”
If you are like me, an average busy ED shift gets fairly stressful by about 4 hours into it, with ambulances ramping and bed block – you know the drill. By this stage on those days, I am feeling a bit like a tightly wound metal spring. Tight muscles everywhere and just stress. Anxious also because wards won’t take patients or clean their beds fast enough for the ED’s needs. Sounds familiar?
At the end of these shifts it can take a full 24 hours away from ED to recover our sense of calm. My partner says that it takes me 2 days sometimes to become normal again. I treat everything at home as a list of urgent tasks, all needing to be achieved at ED pace.
It doesn’t need to be like this. What if there was a way to reduce the chronic and acute tension that we accumulate in our medical lifestyle all too easily?
“OK, enough words, how do I start this?”
Mindfulness is essentially about speeding up our conscious transitions from stress to calm. It is also about becoming aware of our own level of alertness and anxiety, in any moment.
So what are you thinking about NOW? Lists, tasks, maybe some negative self-talk about a case that did not go so well, or….
If you can, do this exercise when/where it is safe enough to do so uninterrupted for a few minutes…say 5 minutes. Yes, of course, this stuff works better if you can put aside 10 minutes (or more) twice a day, but start small. Baby steps.
Take a slow, deliberate breath IN. Feel it flooding through you with new oxygen all around your body. Let the breath out. As you take another slow breath, try and exclude any other thoughts except the awareness of breathing. Let the breath out. Concentrate on a third breath – really observe it and how the air movement feels in your airway, or your respiratory muscles perhaps. Let that one go also.
Do you feel different, even after only three mindful breaths? In mindfulness language, a “mindful breath” is a studied breath. Less tense? Less tightly wound?
So now go back to your “stress” default mode, deliberately filling your mind with all sorts of random thoughts, lists and emotions. Study how you are feeling now, noting the difference from the state you reached after three conscious breaths.
Now, do 5 mindful breaths. In and out. Study the feeling of the breaths. Don’t try and force them or achieve any state of mind. But do try and focus just on the breaths, and count them. Go for ten if you are getting really confident. It is really hard at first!
But notice the difference between the “pre-breathing you”, and the “post-breathing you”.
The message you are giving your body and your emotions is that you are taking back control.
So back to the lists and worries again. Go for it, feel stressed.
And now do the 5 breaths, and focus like anything on the breathing. Yep, it gets quicker doesn’t it? Your speed of transition improves quickly, especially if you practise every day.
Imagine if you could practise every day for 5 or 10 minutes and maintain it. And even a 20- 30 minute practice each week?
And is it that much of a stretch to grab a few moments WITHIN the work day to practise breathing mindfully? And to identify moments where you need to do it, for example after a challenging phone call, or a meeting with a tired relative who can’t visit their mother in ED due to COVID rules? And what if you set aside a few quiet seconds before that phone call, to transition from stress to calm before taking on the phone call, or meeting?
We talk about teaching-on-the-run, so why not mindful-on-the-run?
And the kicker is that as you get some runs on the board, regularly, with mindfulness practise sessions, you will see that your default mode starts to shift from being stressed mostly, to being calm mostly. Things won’t get you wound up. Triggers stop triggering.
I know it works. But don’t take it from me. Try it. It is only breathing. Not that hard.
Next time we’ll talk about what changes anatomically in your brain as you develop your own mindfulness practice.
Take care of yourself and thanks for reading this.
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
“So where is the science to prove the value of mindfulness?”
In short, there is prolific scientific evidence in the research literature of neuropsychology, and a whole interdisciplinary field of meditation science called “Contemplative Neuroscience”. The nexus between modern clinical psychology and both Eastern and Western contemplative traditions, continues to generate large amounts of good quality peer-reviewed data.
Here is one of many..
(see also the links in Article 1 above, especially those of Dr Craig Hassed at Monash University) https://www.pacificneuroscienceinstitute.org/blog/brain-health/meditation-mindfulness- for-stress-reduction/
[and two quotes below are from the above website..]
“Mindfulness training is a widely accessible activity which is deeply rooted in centuries old Buddhist meditation practices. Scientific inquiry into understanding the neuroscience behind this ancient spiritual practice, specifically, “Contemplative Neuroscience” has applied leading-edge neuroimaging techniques showing that regular, mindfulness meditation practice increases aspects of brain function and structure that tend to decline with normal aging. This includes areas in the prefrontal cortex, responsible for organization, planning, and attention, as well as the hippocampus, responsible for learning and memory, all of which tend to decline in size and activity over time. Additional supporting research shows that mindfulness meditation strengthens brain activity and connectivity, psychological well-being, as well as brain volume. These data indicate that meditation can counteract memory issues and general cognitive decline associated with Mild Cognitive Impairment and dementia.”
“Combating regular stress is critical to healthy aging. When not regulated or controlled, stress can contribute to inflammation, [exacerbate] neurodegenerative factors, [cause] excess cortisol secretion, and lead to an overall increase in risk for dementia and cognitive decline.
Meditation can stave off the negative effects of stress, and increase neuroprotective compounds in the brain, such as brain-derived neurotrophic factor (BDNF) and [thereby assist in] boosting cognitive reserve. A 2014 review paper found that amongst 47 well-conducted studies of structured meditation training, short meditation programs of about 8 weeks lead to reduced anxiety, depression, stress, pain and improved quality of life.”
The effects of meditation/mindfulness are related to regularity of practice, and as we discussed in earlier articles this practice can be either as scheduled sessions, or ‘on the run’. Benefits are achieved through both.
Intuitively, it makes sense to schedule in a daily or even twice daily practice session of mindfulness.
Scheduling these sessions is also a statement of how much we value our own mental health, and our own inner growth and development. We are important. We are not just FACEMs, or clinicians, or medical students, or spouses or partners. And the evidence suggests that our function in all these other roles will be enhanced as we incorporate mindfulness into our lives.
So the anatomical changes from mindfulness are related to a diminishing emotional reactivity to stress – the hippocampal nucleus actually shrinks in size on MRI scans of regular meditators – which is another way of saying that we are less likely to operate in fight or flight mode when confronted by situations or people that previously would have triggered this reaction in us. Our brain no longer needs this basal reactive functionality so the nucleus regresses anatomically and physiologically.
Further, our ability to think and react calmly in such situations is enhanced – the prefrontal cortex thickness progressively hypertrophies – which is our calm, executive functioning centre associated with creative and reasoned solutions to events.
Ideal meditation times are something to experiment with yourself; early mornings may work well for some, but I prefer evening. Try and make it nearly every day; if you forget to meditate for a few days, the level reached has to be regained again, certainly in the early stages of practice.
What will also happen with regular practice is that you will catch yourself starting to react in your previous default mode, identify this, and be able to quickly terminate that reaction, and choose to react mindfully instead. Less irritability, less anger, less fear. And this “reset process” gets quicker and automatic, with practice.
Research has shown that becoming more aware of your mental states increases activity in the prefrontal cortex and helps you better regulate your emotional center in your brain (the amygdala). Additionally, the dorsolateral prefrontal cortex (the CEO of the brain) works in concert with posterior regions in the brain to help seasoned meditators strengthen the brain network that allows us to pay attention to a task at hand and ignore distractions.
Above quotes are from https://www.pacificneuroscienceinstitute.org/blog/brain-
health/meditation-mindfulness-for-stress-reduction/
Accessed 9 th September, 2021
“Decision time”
The first step of this journey is that we must decide whether or not mindfulness and meditation intuitively appeal to us. If not, the answer is to do something else for your mental health; exercise, a hobby or sport, for example. But at some time, and it might as well be now, we will all come to this area of our own development, especially once we see how it supports and enhances our lives. But the
timing is up to you.
Commonly, the impetus to start this learning curve about mindfulness may be a health or emotional crisis, when someone has a realisation that they just don’t have their own answers any more. We have probably all talked with patients like that in our ED work, or
perhaps friends, or even faced a crisis in our own lives. For some of us, there is no one specific event or crisis, but the motivation is plain and simple curiosity, perhaps to see “how far the rabbit hole goes”…with acknowledgements to Morpheus, in the film The Matrix.
So, let’s take the red pill, but as we know from our work as ED clinicians, the problem with medication, and meditation, is non-compliance.
“So why do people start meditation practice, and then stop?”
The value, I hope, of an ED Physician writing about mindfulness / meditation strategies for busy people is that I know from experience that the transition from day-to-day brain activity, to mindful and meditative states, is particularly hard for us. So, if we don’t see early results
with our first few sessions, we may give up the practice altogether. But it is especially important to persist, and I believe the strategies offered in these articles will help make the process quicker for you as it has for me. I mainly learnt through trial and error, stumbling
around for ages, until significant breakthroughs occurred. My own experience is that the transition process between these states (‘day-to-day’ vs ‘meditation/mindful’ states) is initially quite jarring and challenging. I think that for us ‘Type A’ types, our brain actively resists the process.
“I think that for us ‘Type A’ types, our brain actively resists the process”
But if we work in persistently and assertively perfecting that transition zone, we can break it down to a smooth process, and then it suddenly starts to make sense. It just takes repetition, like the procedural skillsets we develop and eventually master in critical care medicine.
When we teach junior staff a skill, we break it down into sections. Wash your hands, put on PPE, open up the sterile field etc. Meditation is the same, in the early stages. After a certain level, the intellectual constructs lose traction, and an increasingly experiential subjective paradigm takes over. We will each have our own unique experiences, and some common ones of course, as we progress into the vast world of meditation and mindfulness. But the early rocky stages present common difficulties to most of us, so let’s break it down
and lay out a roadmap to make it achievable for ED clinicians. So, whether your mindfulness practice period is 1 minute long, or 20 minutes long, the transition zone can still be tricky from normal day-to-day consciousness to the expanded,
slow thought patterns of meditation.
Our thinking slows as we do the breathing exercise, or a body scan, and then WHAMMO we are back thinking about shopping lists, and concerns about the future, or that patient with the X-Ray finding that we did not see. At this point, we may feel like a complete failure at mindfulness. But it is not so. “At this point, we may feel like a complete failure at mindfulness.
But it is not so”.
All that is happening is that our brain is resisting being at peace, like a cornered tiger. Calm and peace are not natural states for a lot of us.
But the brain can be trained. There is a heap of good scientific evidence to support this. The secret to transition zones into meditation levels of consciousness is to compare meditation to a smorgasbord meal, where you have a range of options on display from which you create a delectable meal. Not really the same as the usual snatched lunch break in the ED!
“And once you have done it one time, you will speed up the process with repetition. Guaranteed.”
And the real secret to the transition zone is to have all of the options on hand, and quickly change between them if one does not seem to be working for you. Our brain can only focus on one thing at a time, so if we fill the bandwidth with transition zone techniques, our brain
faces a real challenge in dishing up the distractions, the lists, the worries. In this way, as we “flood our brains” with a range of transition zone techniques, we can recall a line used by the Daleks in Doctor Who, “resistance is useless”. We break through to spacious meditation consciousness. And once you have done it one time, you will speed up the process with repetition. Guaranteed. You will also learn what approach works best for you.
All of the great meditation techniques were developed by people who understood the crazy ways in which our brains operate, and think. The various strategies all have the same outcome, to help us centre, and stop the mental chatter of our minds. Next time, we will take a deeper dive into the transition techniques, namely breathing techniques, mantra meditation, body scanning and visualisation. They are not of value in
themselves; they just help us transition through the messy initial stages of meditation to a place we really, really want to reach.
Take care of yourself and thanks for reading this. A/Prof Andrew Dean FACEM Waiver: These articles represent my own views and approach to mindfulness, and do not
purport to be the official view of ACEM. They are not intended to replace appropriate
medical or mental health care, provided by professionals in these domains.
“Defining the terms”
So last time we ended up talking about the main difficulty in all of this mindfulness meditation caper as being the first stages of transitioning away from the frenetic day-to-day thinking, into the quieter, spacious thinking of mindfulness or meditation.
But we need some definitions, because using these two terms mindfulness and meditation together is confusing. For me, too.
Mindfulness has many definitions. Dr John Kabat-Zinn has been instrumental in launching mindfulness in the West; he correctly realised that making these techniques approachable in a modern setting required an apparent separation of the study and techniques of mindfulness from their historical background; in this case, from the Buddhist traditions of meditation that are over two thousand years old.
The term mindfulness describes the conscious development of self-awareness and observation of one’s surroundings, in the present moment. There are many techniques.
Meditation is more a descriptor of the process and methods by which we can enter different levels of consciousness – apart from waking and sleep. There are many techniques and ‘languages’ here also.
Meditation as an idea is less approachable perhaps for our busy minds, whereas mindfulness may be a more accepted term in the Western world.
“But does it really matter?”
I respectfully suggest that it really doesn’t matter which term we choose. The overlaps are so great, and the techniques are so similar.
We need to keep all of this terminology as simple and credible as possible.
“So, what’s this transition stuff he is talking about?”
As a launching idea, the people who developed the techniques of mindfulness and meditation really knew what they were doing; they understood how hard it is for our minds to get though the early stages of learning this. Perhaps like training a race horse, or a
puppy, or an intern in the ED.
We are so used to noise and interruptions and distractibility, and of course all of the emotional reactivity that goes along with having a partly trained mind. We think of ourselves as being disciplined in some ways, but in terms of the mind itself our thinking is kind of all over the place for huge parts of our days.
Sitting down for the first few times and trying to relax or meditate usually fails spectacularly. Some lucky individuals immediately have profound experiences when they learn to meditate, but for most of us, it requires regular practice with plateaus and some accelerated
periods of growth.
To help us pull back on track, as we sit and meditate, there are tricks, and by understanding a few of these at a cognitive level we can use several, if our mind is wandering. Everybody gets distracted in meditation. I will put some diagrams into subsequent articles to explain
that this does not matter.
“I remember The Beatles, don’t you?”
One example is mantra meditation which is used in Transcendental Meditation ™, made popular by the Beatles as they too explored new horizons in their early adulthood. And, perhaps, some pharmacology sessions of a rather different nature to the usual ED Registrar
tutorials.
A mantra is a word, or a series of words, that the meditator repeats. When distracting thoughts come, as of course they will, the person tries to remember to re-start the rhythmic repeating of the mantra, perhaps linking the mantra to an in-breath, or to the out-breath.
Mantras in TM™ are old Indian or Sanskrit words, but any word works. It could be shoelace or defib repeated quietly, and the effect would still occur. Others use words with an emotional resonance, such as love, or stillness. I find it powerful to quietly repeat something like thankyou, which brings in one of the values of mindfulness, which is gratitude. But more on that in a later article.
Mantra meditation is certainly successful as a technique of transitioning. This success is not because of the word or words chosen, but because of the repetitive nature of repeating the inner word sequence. Our mind becomes slowly but steadily prised off its rock, despite its determination to hold on. People use rosary beads, or tap on a table with a small glass at a certain speed, to effect the transition. Repeated lines of prayer have the same meditative effect, and these have been used for aeons in religious meditation and prayer practice.
So, try using mantras. Make up your own. Finding a word that is sacred to you really helps with the whole mindfulness and meditation journey; a dedication to yourself is an essential element. You will likely ‘chop and change’ a lot as you explore what works and what does not, and that is all very healthy.
Next, we have some of the mindfulness body scan techniques, where you sit with eyes closed – or open, it does not matter – and sequentially start somewhere in your body and just observe physical sensations such as weight, muscle tension, temperature, air movement through the respiratory tract etc.
This is similar to the many breathing techniques, where we focus on the sensation of air passing in and out of our nostrils, or throat, or the expansion of the abdominal and chest area with respiration.
These have developed as transition techniques because we simply have to breathe, so the stimulus is there to pull our mind away from “busy thoughts” to something calmer. And likewise there is nothing particularly special about the body scan mindfulness techniques, other than the awareness being easily available from the physical sensory inputs we receive as we sit down in a chair.
They are just techniques of distraction, to help us transition. Practising all of these a few times enables us to use any or all of these, while we ‘wrestle the tiger of distractibility’ in the early stages of learning how to meditate.
“It all sounds pretty hard”.
But it is just repetition. Calm non-judgmental repetition. And we don’t listen to negative self-thoughts, such as “I can’t do this”. Just repetition.
Depending on how “wired” we are, the initial practise sessions may be as brief as a few minutes. With time, sessions of 5 or 10 minutes may not be intimidating.
And as the Oracle in the Matrix films almost said, what really ‘fries our noodle’ with meditation is that the mind gets used to the amazing feeling from mindfulness sessions, and about the same time each day and often in between times, our mind urges us to meditate. If you can escape from your day for even a few minutes to respond to these inner signals, and sit quietly and mindfully, you should do so.
“So what’s coming next?”
Next time, we will look at other techniques of transition, including the use of music, metronomes, guided meditations, flashing light devices and visualisation. It all sounds a bit complicated, but the good news is that once we master transition to meditative states, it does get easier. The focus on the transition zone is really important.
Take care of yourself and thanks for reading this.
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not
purport to be the official view of ACEM. They are not intended to replace appropriate
medical or mental health care, provided by professionals in these domains.
“It’s all in your imagination”
The “meditation industry”
The transition into meditation is the hardest part for all of us at first, and because of this, a whole “meditation industry” of various types of meditation aids, devices, books and music has arisen to help us out. And, no doubt, to create commercial opportunities for the creators. In the interests of transparency, I must declare myself as a participant in this, having written a book on the topic.
Once we have practised enough transitions from waking state to meditation state, we begin to build up our own library of ‘cues’ about our own individual transition process. And then, we can tune into those cues – or lack of them if we are a bit “scrambled” – and by using our own biofeedback, we can “nut it out” for ourselves. There is a bit of stumbling around in the dark for a while, but persist, because the fog clears, and the whole thing then starts to motor along quite nicely.
Once we have experienced what it feels like we can steer the same route again when we have our next practice. Navigating by feelings sounds so corny, but that is how it seems to work.
“I don’t really know why mindfulness has to be so difficult to achieve..”
I don’t really know why mindfulness has to be so difficult for us to achieve in our fast-moving lives, but it seems to be the case. At first. But with repetition and trial and error we learn about our own inner signals of what the different states feel like. Let’s use an example.
What’s your favourite relaxation / holiday activity? What is your absolute best experience you have ever had doing that? What did it feel like when you were completely “in the zone” during that activity?
Now do a simple three mindful breaths exercise, and re-capture that “zone” feeling, focussing really hard on recalling the feeling. You will probably notice after a few seconds that a part of you has “gone there” into that feeling, and your physiology may be shaping itself to exactly how it was, when you were undertaking that activity. Breathe for a minute and explore that feeling of whatever that great moment was for you. Then, slowly come back to now.
“I have just tricked you into doing your first visualisation..”
I have just tricked you into doing your first visualisation, or maybe not your first for many of you. Imagery creates a physiological response. And the meditation industry realises this, with the proliferation of guided meditations, to music backing tracks often. These aids help us to conjure a visualisation, with the brain falling into line, slowing our heart rate, slowing our breathing and letting muscle tension go. And all because of the induced imagination imagery within the visualisation.
So, we can rely on an external trigger for visualisation, like someone else’s voice telling us what to imagine, or we can do it for ourselves.
“Imagination came easily to us as children..”
Imagination came easily to us as children, as we delved into play and inventing stories effortlessly.
But, with the seriousness of school, and even more so, of medical school, it was easy for us to become unimaginative. But we can build up this shrunken muscle with repetitions, just as we do in the gym with all of those biceps curls (well, this is me imagining here!).
Imagination and visualisation are certainly powerful in meditation practice, but as with Rome, meditation was certainly not built in a day (with only a few sessions before giving up), and there are many roads (techniques) which lead to the same destination.
Having a few techniques ‘dusted off’ for meditation transition is a bit like knowing a few sedation drug combinations for use in the ED. If one doesn’t work, you just pivot to another technique.
And the repetition is reinforced further by using other aids such as (1) same time of day for mindfulness practice, (2) same chair or room in the house, (3) same simple dedication and preparation for the session, and (4) allocating the same amount of time each time you practise. The brain gets the message that you are serious, and it complies.
”The brain gets the message that you are serious, and it complies”
The exciting reinforcement of successful transition achievement comes when we experience our first cool meditation experience. A completely new and different level of consciousness, which feels just great for those moments, and it was all our own work.
And while it is not the aim of mindfulness to clock up “experiences” per se, travelling through the levels of meditation gives us encouragement that we actually can be successful at transitioning into these states using our own reproducible, and ever quicker,
methodology.
“What about the biofeedback headsets and glasses?”
As I said above, all of these tools support our entry into transition, and are useful. But, thankfully, we can quickly go beyond the need to use these once we start to really build up our inner list of “index cards” about how each stage of mindfulness feels. We write our own
map.
So, you may have bought a Muse, or a pair of Deepak Chopra flashing light glasses, as I did, but I don’t use them now because I just don’t need to. And you won’t either, and the music player will probably stay switched off once you really understand transition, your style.
“Touching on the infinite”
The haunting sound of a shakuhachi flute conjures up images of samurai warriors training, and Zen Buddhist monks meditating, in the forests or snow on a Japanese mountainside… Some sounds just have a magical ability, in most of us, to transport us to another level of “in
the zone” awareness. Some call this “touching on the infinite” within us.
As I said, there are many roads, along this very special journey – which is, among other things, about re-establishing your inner calm and balance – despite the noise going on all around you.
Thanks for reading this, and take care of yourself.
Next time we will look at the idea of “signal to noise” and some concepts for how we can better focus on the real signal, and trim out the distracting noise. Mindfulness comes into its own in busy and messy ED situations, and can reduce stress levels and burn-out.
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not
purport to be the official view of ACEM. They are not intended to replace appropriate
medical or mental health care, provided by professionals in these domains.
“Signal to Noise”
An early compelling outcome from regular practice of mindfulness or meditation, call it whatever you prefer, is that we begin to sense that we have an unexpected executive capability to control the whole cacophony of our thoughts and emotions. By and large, our constant firing of neural impulses is shaped by our past. Mindfulness reawakens a dim memory that we can affect the present, and that it doesn’t just randomly happen to us.
“Mindfulness reawakens a dim memory that we can affect the present, and that it doesn’t just randomly happen to us.”
The influences that shape our average brain activity include such predictable culprits as our childhood experiences, the emotional patterns of our early family life during our formative years, a few disasters or momentous events along the way, and of course the daily conditioning of the people we live or work with – they influence our reaction patterns simply because we spend time with them. So, our family or friends are enormously influential on how we react to events, and how we instinctively dive down emotional rabbit holes, positive or negative, when an event or “trigger” happens to us.
In audio technical talk, there is a term called “signal to noise ratio” which refers to the amount of fuzzy static that disrupts a clear signal. Peter Gabriel described it in his brilliant song called “Signal to Noise”, from which these following lines come:
All the while the world is turning to noise
Oh, the more that it’s surrounding us
The more that it destroys
Turn up the signal – wipe out the noise!
So much noise, so much emotional reaction. There is a societal disapproval, certainly a mainstream media disapproval, of calmness, of quiet reflection, of equanimity amidst the noise and haste of “Desiderata” fame.
And, the rest of the opening stanza in Desiderata reads: Go placidly amidst the noise and haste, and remember what peace there may be in silence.
It is surprising how large an obstacle this fundamental belief seems to be: that we can actually take control back from the maelstrom of emotional reactions that forms the majority of our waking thoughts. We can become quiet. We can return to calm clarity.
“We can become quiet. We can return to calm clarity”
The other element in that quote is the idea of going placidly (calmly) amidst the noise and haste. Not escaping, not running away from our lives, but learning how to (1) reliably reach calmness in ourselves, using mindfulness or meditation techniques, and then (2) going right back out into the fray, moving calmly amidst day-to-day events that hitherto would have ‘triggered’ us emotionally. Our effectiveness now is enhanced, because our inner world is calmer; we can quietly hear the ‘signal’ from our intuition about the right thing to say, or do, in any situation. And, the ‘noise’ is no longer dominating our awareness and dragging us along with it.
“Fine words, but…”
Part of the effect of watching our breathing, scanning our body and muscles, in the mindfulness exercises, is that we build a type of early warning radar for detecting ‘imbalance’. When we recognise that we are tensing up, we are then more likely to immediately do the thing that restores us to balance. The mindfulness solutions to stress in any moment are not complex. By practising regularly, both in ‘scheduled’ sessions of mindfulness, and in ‘mindfulness on the run’ moments at work or during our other daily activities, we build the reflex ever stronger. This stuff becomes a mostly automatic response to situations that previously would have us reacting with anger, irritation, anxiety or even reactive depression.
“Let’s practice this mindfulness again …”
Start with a familiar image…
It has been a massive day at work, with over-capacity waiting rooms, and bed-block stretching nerves and energy levels. It is finally ‘go home time’, and you change out of PPE into civilian clothes, and make your way to the staff car park. A busy home with all the issues of the day awaits you, and you are feeling like an over-tightened spring already.
As you sit in your car, quite safely in the car park, let’s do a “reset” mindfulness exercise, a ‘time out’ just for you, before you drive home…
Close your eyes or keep them open if you like, and just stare at something and let your eyes rest from the constant movement of the shift in the ED. Keep all your muscles still.
Follow your breath.
Breathe in, then out.
No need to force it; the smoothing and slowing of breathing happens automatically if we let it.
Just watch your breath, in a detached kind of way,
as if you are standing in the shallows at the beach watching waves rolling in.
With each breath out release some aspect of the winding of your inner ‘spring’. Perhaps
identify a list of the day’s stresses, and work through the list as you breathe slowly.
Let them go.
Feel yourself moving towards the ‘calm you’, increment by increment, with each breath.
Breathe out some tension from shoulders, or jaw muscles perhaps, or let your tension
headache move out and away, with the breathing pattern.
If you get distracted, don’t worry; just recognise this, and simply recommence the pattern.
Once you have done a few minutes of this, give yourself a break and just have some unscripted
mindfulness time, not trying to focus on or do anything, and simply enjoy the ‘unwound’ feeling
that you have just created.
Perhaps take 5 more minutes, or even 10 minutes if you feel comfortable, then ease your mind
back into the mundane world of carparks and commuting, and another normal evening at home
with your loved ones…
But you have changed, and you will go home different, with a new, mindful element awakened in
you as you engage with the evening.
Thanks for reading this, and take care of yourself.
Next time we will look at mindfulness applied in the workplace, with some examples, and
go over the concepts about how the hurdles to mindfulness are essentially transition zone
problems, and the strategies are simple – if only we would remember to practise
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not
purport to be the official view of ACEM. They are not intended to replace appropriate
medical or mental health care, provided by professionals in these domains.
“Waiting to arise”
“Mindfulness is not just about you”
To summarise the story so far, mindfulness and meditation are tools that help us to
- react less to triggers,
- be calmer,
- relate better to others
- develop a clearer sense of who we are, and our role here.
Popular mindfulness and meditation books and self-help courses emphasise these as benefits to the individual, but few contextualise mindfulness in its greater function, which is to equip us to be stronger and more effective in helping others, and through providing such help we of course assist ourselves. The weary world needs your strength, and mine.
In other words, mindfulness has a social function, a contribution to those around us.
How does this work, in particular, in relation to hospitals or the ED?
“What’s he talking about? A mindful workplace?”
We intuitively know that colleagues radiate an energy when they enter a meeting, or a room in the workplace, or any room for that matter. Stay with me on this. Most people who are in a reasonable level of balance emit a neutral kind of energy, and we are hardly aware of that. Hopefully we can do even better than that, and radiate a really positive energy to our colleagues and patients.
But some individuals who have significant antisocial tendencies will enter a room and the other people in the room may likely feel unease or discomfort. The extreme form of this would be someone who is drug affected from amphetamines – they create a massive challenge (let alone the physical risk) for the ED staff caring for them, just because of the pattern of energy that radiates from a drug affected person. Another example is the frustrated or aggressive patient or relative who is reacting against the delays to treatment in a typical overcrowded ED. We feel their bristling and perhaps even threatening energy, and to be effective we need to be extra mindful of this in the way we communicate with them, in our verbal de-escalation efforts.
“..emit a mindful energy of care..”
Mindfulness helps us to create the opposite situation within ourselves, a calm centre, an eye of the hurricane if you like, and we can then be emitters of a mindful energy of care, empathy and compassion in the midst of a noisy and challenging workplace. This is the inner workspace from which highly creative and effective interactions with other people arise. I will come back to this again, the idea of a mindful parallel inner narrative.
In other words, we first need to create or access a mindful workplace internally in ourselves, and then effective communication just happens. We say and do the right thing. Having said this, in escalating situations with aggressive behaviour, staff and patient safety still remain paramount, including the use of physical or pharmacological restraints as needed.
The link to CommLabs @ LITFL.com
I have just discovered the excellent CommLabs posts by Dr Hayden Richards on LITFL.com, which address this whole area of emotionally intelligent communication, in the midst of challenging ED situations. These skillsets could certainly be described as mindful communication. I recommend watching Hayden’s CommLabs articles, and his YouTube videos on expert interpersonal communication. The lessons apply generally, not just in medicine or the ED.
So, of course, you’ve guessed that the topic today is ED culture, and awakening ourselves to the powerful contributions that we can make to culture, as mindful emergency medicine professionals. Every staff member is included in this, not just the FACEM or the medical team.
“Emulate the best, not the worst”
I would not be the only teacher of trainees and students in the ED who says to them: “follow the example of the best doctor you can identify, because they will teach you what you need”.
Of course, we need technical skills champions in the ED, who are expert in the cognitive and procedural skillsets, but also we need champions in the non-technical skills of communication and great leadership – and we need champions in mindfulness. Every ED or workplace needs such role models of how it is really done well. A good workplace culture grows into good workplace health, and is the result of constant nurturing.
And as we know from our children, or trainees at work, we are measured on what we do, rather than what we say. From here on, as you start your own mindfulness journeys, there are no holidays. Every conversation matters, every person you deal with. And do students of mindfulness sometimes get it wrong, and revisit conflict and get into occasional arguments? Of course, but our overall default state moves towards reduction in conflict and harm.
The “values” of mindfulness
Hospitals and many companies have mission statements, values statements and the like which hopefully translate into the level of service they provide to customers, or in our case, our patients.
It does not always work.
Some of us will have roles in administration, to try and optimise policy and obtain enough staffing and resources to support the “front line” team, as they endeavour to deliver on the values of care.
Others of us just work in the front line. Regardless, each individual in the hospital has a role to play in convincingly delivering on the hospital’s values.
The values that enrich our workplace are things like
- patience
- gratitude
- appreciation
- respect
- being attentive in the moment
We can’t “do mindfulness” for ourselves, and not try to engage with our fellow humans in a mindful way. Any inconsistency in this simply cannot be sustained. Mindfulness is all about our dealings with others; it is a binary gift that must be given away to be received.
The idea that we can separate out the elements of our lives (work, family,..) and have acceptable different behavioural frameworks for each (“s/he is a bully at work, but lovely to her/his family at home”) makes no sense, and as we explore mindfulness such dichotomies become glaringly apparent, and in need of resolution.
And this brings us toward the true mission statement for you, for me, for all of us. We can use the tools of mindfulness and meditation to reshape ourselves, to bring health and joy not only to ourselves, but also to all of those other people in the spaces we inhabit, in our day to day lives.
“The two triggers for getting started in mindfulness are pain, or curiosity”
We will get back to the mechanics of mindfulness in the middle of our working days in the coming blogs, and then look at the longer practise sessions of meditation in more detail.
And even though I wrote in the early Mindfulness articles (for example in #1) about how this mindfulness caper may not be for you, in a way, it always is. For all of us. The only variable in this that we can control is the timing.
At some stage, you and I and every person will have to work all of these concepts into our/their lives. The two triggers for getting started in mindfulness are either pain, or curiosity. The concepts of elective surgery and emergency surgery are well known in healthcare. Mindfulness is similar. My question is, why leave mindfulness until the wheels fall off the cart? Why not start now?
“…all your life, you were only waiting for this moment to arise”
And so we come to the close for this week, with another line from a song, this time from the song Blackbird, by the Beatles. You indeed are a unique and special part of all things, and all your life, you were only waiting for this moment to arise.
Thanks for reading this, and take care of yourself.
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
The mechanics of mindfulness
Mindfulness is like cookery
The time that we allocate to activities influences the outcome, and our skill level in that activity. This applies to cookery, and to our domain specific skills such as IV cannulation.
Mindfulness is no different; skimming through a mindfulness book in a bookshop is not the same as setting aside 10 minutes a day, and remembering to create brief mindfulness sessions “on the run” while at work, or on the train commuting, or playing with your kids at a park.
So, in an average work day, let’s identify the moments we could use to help build mindfulness.
Mindful in the morning rush
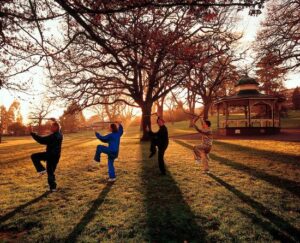
Scheduling in slightly earlier rising, when the house is at peace, creates a chance to do something specifically mindful, whether it is a proper meditation session, or slow walking, or tai chi or yoga. Animals and gardens are ideal mindfulness activities, but walking a boisterous young puppy perhaps not as ideal..
Even just a few minutes of deliberate slow walking, with some basic breathing focus, is like opening a door in our mind. You would probably know of ‘walking a labyrinth’, which is certainly meditative, which is one example of how very slow and silent walking can be very calming. Walking slowly anywhere works, but make your movements at half-speed; it sounds crazy, but just try it once for a few minutes, and notice what it feels like. You can wash mindfully, or comb your hair, or brush your teeth, or eat mindfully. All it takes is some imagination, silence, and a lack of interruptions. The challenge is to maintain this in the thick of things, but it comes with practice.
Mindful commuting?!
While on the subject of commuting, driving a car is not a safe time to meditate, but it does however provide some excellent mindfulness opportunities – to do with Zen flow, trust, and plenty of forgiveness practice, involving our reactions to drivers demonstrating “sub-optimal driving skills”.
Certainly, commuting on a bus or a train both create practice time, for breathing, stilling thoughts, letting go emotional reactions, or just scanning our thoughts as they randomly float by. There is no need to close eyes to practise mindfulness; just fixate on something in the lower visual field, and keep your eyes fairly still as you focus your concentration inward, on breathing, for example. It is just practice, and this is another example of how transition zone practice becomes progressively easier and faster.
Mindful moments in the hospital
This is all leading towards a discussion of the two narratives in our mind, the ‘out there’ one which we all need for busy concentrated cognitive activity e.g. running a ward round in the ED, and the ‘in there’ parallel mindful narrative that we learn to strengthen progressively with practice. It all sounds a bit like a split mind but it is not really. Perhaps it is more akin to developing an under-utilised part of our mind.
Examples of when you could hold your eyes still, drift into mindful breathing and awareness, while fully conscious and quiet, include waiting for coffee, watching the Urinalysis or VBG machine processing your test, waiting for people to arrive at a meeting or tutorial, walking to the carpark, or along a corridor to the Imaging Department…they need only be brief interludes, perhaps a minute or two, and you prove to yourself that you can do this stuff, and fairly quickly at that.
If you have the luxury of an office and some quietish non-clinical time allocation, well, where do I start?! Plenty of chances.
“Micro-silences” through the day
We think often that we are our noisy mental chatter, and that our swinging emotional reactions are us.
By working on identifying and creating even very short moments of mindfulness right in the middle of our busy days, we build the skill of “micro-silences”, where we realise that what is happening on the surface of our ocean, so to speak, is not the entirety of the ocean.
This skill of micro-silences also helps prepare us for difficult conversations, where our communication needs to be free from attack, focussed on listening, and open to creative solutions. Hayden Richards covers this whole topic so well in his blog, CommLabs.
The tiny silences that we sequentially create, in all sorts of unlikely moments in our day, have the effect over time of rebuilding us. They help us to reshape our default mode towards greater levels of equanimity, forgiveness, calm amidst chaos, and reduced abrasion in our interpersonal relationships, both at work and at home.
The “longer” practice sessions
Mindfulness ‘on the run’ is really useful, and extends our influence in the workplace, and has positive effects on others around us. This is evidence-based from modern research in neuroscience.
However, much faster progress will come if a session of even a few minutes a day is set aside for a sustained practise of the transition techniques we have already covered. Sitting in a comfortable chair, having freedom from interruptions, and a regular time to practise if possible, sets the scene for letting ourselves really ‘go deeper’ into a deep relaxation state, or mindfulness, or meditation – the wording is not the key thing.
These sessions are for experimenting, to try the various transition methods – some of which are listed here:-
- breathing observation,
- slow movement, or a walking meditation
- body scanning, of muscle tension and other visceral awareness
- mantras
- music
- biofeedback devices
- concentrating on a picture
- focussing on a single light source
- reading ‘affirmations’ that resonate with you
With each method, really focus on what body and mind changes are occurring during the session. If it feels uncomfortable, stop, and do something different. Expect some resistance at first, especially for us ‘wired’ emergency health professional types. It passes.
Use other materials as catalysts; for example, you might find YouTube videos on the topic of mindfulness – there are some millions of them at last count! You may be drawn to buy and read a book which reaches you. Some people keep a diary of their mindfulness sessions. You could join a group, either on-line or face to face.
Many roads
There are many roads to mindfulness. Each person’s study materials will be different, and the pace of the semesters will be tailored to the individual, so to speak. And we can certainly withdraw from the ‘course’, and defer our studies for a few years. My own journey in mindfulness has been of a rather stop/start nature, until the past few years. Now, it is a central focus. Your own road to mindfulness will be unique to you.
And talking of roads, every morning in cities across the world, as traffic surges and blares incessantly, one will commonly see small city parks with groups of tai chi practitioners, who provide a brave counterpoint of calm to the noise and smoke nearby. Slow extension of gracious arms, fingers loose, with synchronised heel turns and sliding hands, moving into a ‘brush bird’s tail’ pose.
We can also be that brave counterpoint of calm.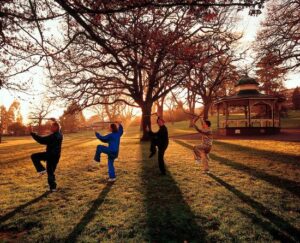
Accessed 14th November, 2021.
Thanks for reading this, and take care of yourself.
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
Ocean explorations
To recap:-
- Mindfulness can be conceptualised is as an ocean,
- When we are active in our working ED day, we are metaphorically swimming in the surface waves, racing around, engaged in our left brain with conversations, clinical reasoning and analysis of information.
Swimming
By looking out for small opportunities, we can do ‘mindfulness on the run’, and briefly access the quieter layers of the water just below the choppy surface waves, using transition strategies such as micro-silences, and short moments of deliberate slow breathing, or slow body movement.
With regular thinking about mindfulness, and some practice also, you will likely find, as I did, that this becomes a whole new way of operating for you.
Mindfulness does not get in the way, but it helps with personal stress management, having difficult conversations, resolving frustrating issues at work, and with family relationships as well. You will think about mindful approaches instinctively, and even if you completely forget what you have learned (it is pretty common!) and react in “the old way” in some situations, progressively you will remember your mindful self, and it soon becomes an automatic skill.
There is no way back to the old you, and why would you really want that? It could be described as a one-way door.
The deeper dive
But the interesting stuff comes in with scheduled mindfulness practice sessions, when we learn about what capabilities our brain has to “go deep” into meditation states. The inner explorations do become fascinating in themselves, but are also very effective at restoring calmness and balance. So if you are interested, how does one deepen the meditative state, in a no-nonsense description?
Using the ocean analogy again, the most turbulence is in the upper layers of the water. As we settle into a mindfulness session, we drift down, but are just as likely to be distracted, and float back up to the normal wakeful thinking levels for a time, until we notice this, and concentrate on our breathing, and drift down again to slower thoughts and real stillness.
It takes a bit of practice to get the early transition techniques established, to access the first layers of meditation states. Distractibility is our trademark, it seems, particularly for people who have a strong intellectual component to the way they live and work.
But every second of deliberate mindfulness makes a difference in terms of creating new connections between our dendrites and neurones in our brains. New neural pathways are opened up. And every time we reinforce this new learned behaviour, it edges closer and closer to becoming a reflexive way of reacting to any stressful thoughts or emotions. In the language of the neuroscience literature, we are incrementally (and irreversibly) shifting our default brain settings away from reactivity, anger and anxiety.
The practice
Get yourself set up for a mindfulness session.
Adjust your position on the chair or cushion.
Eyes closed.
Watch your breath.
Slow your breathing a little, but mainly just observe it.
As everything quietens, study what sensations are arising, and fading away.
Try and maintain this for 5 minutes, then return to normal waking consciousness.
The theory
Focussing on the differences in the levels of mindfulness helps us to build a roadmap of this domain.
Descriptions of the levels in words is helpful. Fir example, waking consciousness could be called ‘Normal Noisy Thought’ or NNT, and as you go into a mindfulness practice session your thinking slows and oscillates less between multiple threads of thought. I call this ‘Slowing Spacious Thought’ or SST for short. You will quickly be able to compare the feeling of these two different states.
As you breathe mindfully, your mind in those moments literally cannot sustain NNT pattern. It automatically changes more towards the SST mindfulness thought patterns. These transitions in brain activity during meditation can be observed as increasing coherence of the brain wave frequencies on an EEG or fMRI scanner.
The timing, as they say, is everything in Cardiology, and also in mindfulness. The easiest practical options for mindfulness sessions are often at the beginning, and the end of the day. On waking, my experience is that I need to get fully awake before I practise mindfulness, or else I tend to gravitate back to sleep and doze off. Likewise, at the end of the day, if we try to meditate lying down in bed, especially if we are tired, sleep usually takes over. So the sitting position, with a clear head, is the best preparation for mindfulness or meditation. If you have spare time during the day, you can meditate anywhere and anytime. Avoid excess alcohol and heavy meals in the lead up to mindfulness practice.
As for the length of mindfulness practice sessions, start slowly and work up to longer sessions as your mastery of the transition process consolidates. Five minutes is fine, and gradually your brain will become a better student of sitting still for more extended periods. An hour of meditation is not for the faint hearted, but rather for the experienced meditation aficionados.
With each session of mindfulness, you need to develop acute observation of what each level feels like. Start with what normal waking thinking feels like. That is easy. Then observe how your muscles feel as they completely lose all tension, and flop to a completely still and comfortable position. The initial discomfort and wriggling around that we all experience on entering meditation just fades away, and you will come to a point where your body is completely still, and completely comfortable to stay there, for a time. It will feel very unfamiliar – but very comfortable at the same time.
Athletes develop muscle memory, and mindfulness sessions are similar. You will develop an ability to rapidly transition through the early stages of distractions, and you will look back and wonder why you found it so difficult.
The composite feelings of the different levels of meditation are like signposts of sorts: for example, one level of meditation can be characterised by complete muscle relaxation, slowing languid thinking speed, and less spatial awareness of body size and weight. When you stumble into this space, as you will by chance one day fairly soon if you practise enough, the feeling of that level will be stored as a memory. Next time, in a mindfulness session, by pulling up the memory of that particular level of meditation, your brain will start to ‘go there’.
As you deepen, thoughts can be used to guide you further into stillness. But those thoughts need to be short thoughts, often single phrases or even single words, just quietly repeated to hold back the distractions which would pull you up to NNT levels again.
For example, as you settle and drift down, try saying mentally: ‘deeper, deeper, deeper..’ every few seconds, or to frame your mindfulness session in gratitude, you could say something like: ‘thank you, thank you..’, and eventually shorten to single syllable words. It all works. The word does not matter so much as the dedication or intention behind the whole practice session. The spacing between the words gets longer as you deepen, and then you realise that you have just had a few seconds of absent thoughts while being very still, and completely alert. Very cool.
The trick to deepening meditation levels is to be gentle and not to force things. Forcing brings emotions into the practice, which haul you straight back to NNT levels. Don’t force things on the descent, and don’t force things on the ascent back to normal waking NNT states. Jumping out of a mindfulness session to full alertness is jarring. It does not do you any harm, but it takes a few minutes to recalibrate and you may have a headache for a few minutes.
So set a timer, or use one of the meditation apps, which play a chime at the selected finish time, and give yourself a few minutes as you come out of meditation to stretch your limbs, open your eyes slowly, and gradually rise back to full alertness. This also becomes quite fast, as you continue a regular practice.
And at the end of each session, give thanks for what you have experienced. Gratitude is all over the mindfulness literature these days, for a very good reason. It teaches us a humble appreciation for the many gifts we have and will continue to have.
Mindful Leadership, and some other concluding ideas
In discussions about meditation and mindfulness, people use terms like ‘downloads’, to describe the spontaneous thoughts and bright ideas that arise during or after meditation sessions. Creative solutions to problems also commonly present themselves after we have had sleep or rest. Developing the discipline of daily mindfulness will give you an increased confidence in these processes. Try it for yourself.
Leaders in hospitals and EDs commonly need creative solutions to problems. Trying to solve issues in an inner atmosphere of irritability or resentment is difficult. Developing mindful leadership attributes in ourselves makes so much sense, especially now.
The strongest leaders come from the values of care, humility and trust in their colleagues.
As you go down the mindfulness path, everything softens, and out of nowhere you will find yourself pondering values and concepts such as patience, forgiveness, generosity and trust as your inner ‘reframing’ develops momentum. We are, each of us, destined to become a gentler, more caring version of ourselves, it seems. Mindfulness is certainly not the only roadmap, but it is a way.
Thankyou for reading this, and take care of yourself
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
Teacher training
To recap:
- Mindfulness for busy people is a discipline and an attitude, supported by regular practice
- It is like a lens, through which we can view each event in the unfolding day
- We can use mindfulness to transform our unhelpful reaction patterns
Front-line ‘transformers’
‘‘There’s no time for toilet breaks, let alone mindful breaths…and as for that mindful workplace stuff – give me a break!’
That kind of comment may sound familiar to most of us. And there is no doubt that through our working days in the ED, we are ‘on the go’ from shift start until much later, with breaks truncated, and going from patient to patient it may seem as though we are just in a kind of survival mode.
So, what’s the relevance of mindfulness to this…
Let’s maybe rearrange the end of that sentence to ‘a survival of kind mode’.
A very few people working on a shift with an attitude of kindness can transform the enjoyment of the shift for everyone, and most importantly, for the patients’ experience. Those people may be medical staff, nurses, administration or reception staff, or environmental services and catering staff. The influence of our attitude and energy that we radiate throughout our day goes way further than we imagine. In distant areas of the hospital, staff who you may have never met will be influenced by you, and so in turn will their care for patients or their role in the hospital be affected, either positively or negatively. I know this, from my own clinical life as an emergency physician.
If that number of ‘transformers’ is only one person, the power to positively impact the energy and resilience of other staff members is still significant, but if two or more are working actively to support everyone around them, to help steer conversations away from negativity, and to demonstrate consistent compassionate care, the cumulative positive effects can be enormous.
‘Show me the data…’
Many people working in the front line of emergency medicine already know this, and are taking action to become the transformers within their workspaces.
I recommend the resources of our FACEM colleagues at WRAP EM, https://www.wrapem.org, who are developing ED wide mindfulness, wellness and resilience innovations, and other Australian EDs have introduced ‘appreciation notice boards’ and related initiatives, to help acknowledge and strengthen the culture and morale of their teams, for example the Learning from Excellence (LEX) programme in the Royal Hobart Hospital ED < https://vimeo.com/299345500 > .
These examples of ‘team mindfulness’ do of course overlap with individual mindfulness, but what is exciting is that these programmes create positive change across the wider ED and hospital workforce, thereby developing increased whole-staff wellness, stress resilience and a healthy team culture, using principles derived from mindfulness.
“That stuff is the Director’s role…”
It is easy and appealing perhaps to think that we are not really responsible for nurturing every other person in our ED or workspace, and that some conversations matter more than others, or some interpersonal interactions are more important than others. Mindfulness and meditation show us that we cannot hide behind our titles, labels and other artificial classifications, particularly in the way we relate to others. Delving into ourselves usually brings up an uncomfortable awareness of any inconsistencies and half-truths that we need to transmute into more authentic patterns of relating to others.
Change in culture within an ED (or anywhere) requires a small dedicated nucleus of people, and while it is certainly important for Directors and Managers to be aware of emotional intelligence and mindfulness, there is no reason why any person or people within a workspace cannot become transformers and initiators of mindful culture change. You can be the change you want, as the saying goes. The quality of your light affects everything around you, in ways you may have never believed possible.
Mindfulness practice session
In one of your scheduled morning mindfulness sessions, try doing the following exercise to demonstrate what we have covered so far…. Even better, perhaps discuss this concept at a ward meeting or planning session.
Preparation time: 10 minutes
Level of difficulty: Easy
- Settle into a chair for the session
- Use a breath awareness or another transition technique*
- With each out-breath, imagine you are sliding further down into complete stillness
- Notice any distractions that ‘pull you back’
- When you notice that you have been distracted, simply resume the transition technique
- When you realise that you have reached that ‘bottom of the ocean’ stillness, do nothing else
- Just sit at this level and enjoy that slow, spacious thinking
- Now see yourself as being deeply responsible for distributing this stillness, and a powerful level of genuine care, to all the people who you will see today after this session of mindfulness
- See yourself as a transformer, taking the inner qualities that you are exploring for your own growth, and giving them away freely to others you will meet
- As you breathe at this stillness level, see yourself opening up progressively to operate in this new role
- Be open-minded about this exercise having a real and positive effect on those around you as you undertake your work today
- When you are ready, slowly come out of the session, using your breath and beginning to move your muscles and limbs
- Open your eyes and when fully awake, resume your day
- Thankyou
*For information on transition techniques see Article #6 and #7
“I can’t teach this stuff”
We teach in every moment, as we walk down a corridor, or show respect to other drivers on the road. We teach our students and colleagues when they see the way we handle delays or other staff at work. In the ED, we are always on open display, and are observed by others continuously.
If we allow ourselves to attack a colleague verbally, or deliberately embarrass someone, we are teaching.
If we use offensive or sexist language, we are teaching.
So, with such public exposure and educational authority, we have a choice to make.
Do we pretend that we don’t need to be consistent at all times, or do we jump into the idea that we are always teaching, always influencing culture, always being visible role-models, and always demonstrating what kind of transformer we want to be in our workspace? And do we apply mindfulness concepts not just occasionally, but all the time once we realise how widely these concepts are being introduced across work spaces?
Of course we are teachers, and you and I also, whether we like it or not.
Seeing yourself as a custodian
Seeing yourself as a custodian of the whole work space (or the whole ED) creates a sense of responsibility for all the people who come into your ED. What you do matters, and it sure is noticed. With mindfulness strategies, and some regularity of practice, you will enhance your own stress resilience and wellbeing to such an extent that you will feel you do have enough to give back to others.
If you are burnt out, you will be a lousy custodian and ED role-model. Do what you need to change that, back towards balance. Maintaining inner balance is homework we all must do.
And then, you will become the change you want, the role-model who lifts the spirits of all the people you meet at work. Others will certainly notice that you radiate something special, but they can’t quite put their finger on what it is…
This is all possible, amidst the noise and haste of our ED working lives.
Thankyou for reading this, and take care of yourself
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
Choosing the right frame
Under pressure
What a time to practise emergency medicine. Pressure and stress are familiar companions in ED work, but within reason. Conversations with senior colleagues in recent times show a picture of a system under great strain. Our individual management of stress is clearly just one part of the needed system-wide resourcing solution.
But as we lobby for system change, and try to keep going, our individual career sustainability also comes down to how we view and process stress, and how we interact with our colleagues and patients. Are most of those interactions positive, or do we feel emotionally bruised from conversations regularly? What is the overall picture, for us?
Reducing collateral damage
One of the learnings from mindfulness is that we are ultimately responsible for each of our conversations, each of our reactions, and each of our emotional responses. How we relate to others (in a nurturing way, or otherwise) determines not only their likely reaction to our words, but also our own level of happiness.
Taking out our own stress on others may seem easy, as a release valve effect, but the harm it does is ultimately to ourselves. How many of us (I include myself here) have later regretted a comment or conversation, in which we left someone feeling judged and diminished?
This cycle of ‘hurt’ / ‘secondary hurt’ / ‘collateral emotional damage’ is familiar to staff in hospitals, as a consequence of conversations with other colleagues. It need not be so. The level of external stress is not the root cause. It is our reaction to stress, and our external projection of that reaction, that causes the harm. And we can modify that final stage of the cycle, and avoid saying things that cause damage to our colleagues or patients.
It is our reaction to stress, and our external projection of that reaction, that causes the harm..
Reframing the choice
We can change our perspective about a situation, and here is a simple example of how we can use mindfulness to do just that, and leave the players in a positive state rather than a defeated state.
How we approach a difficult IV cannulation is one analogy of how we can approach every day mindfully, and indeed every moment in that day. The outcomes can be so different if we try to do this.
Let’s take the example in the ED where you as the senior doctor are asked by a junior doctor or a nurse to help with a difficult cannulation. The ED is overloaded, you are understaffed today, the junior medical staff are aware of the pressure…familiar stuff.
There is probably a feeling of irritation forming right about now…thoughts like
- “Why can’t these juniors insert their own IV’s?”, or
- “This is the last thing I need today”
Here there is a choice. Mindfulness highlights the choices we actually have, in the lead-up to our externalised reactions.
What is the choice?
You guessed it. A choice between an ‘irritable’ reaction internally and externally, versus quickly moving into the more mindful ‘nurturing and illustrating IV technique’ mode, albeit a quicker tutorial than usual, because of the current ED overload situation.
What are the consequences of each reaction mode?
Two reaction modes
If we are in irritability mode, we are
- more likely to fail to cannulate the patient, because we are not focussed on the cannulation
- more likely to create a ‘fear of asking for help’ in our junior colleague
- missing a positive communication opportunity with the patient, and an opportunity to gain clinically relevant information
If we move our reaction to mindful mode – in this example we could also call this the ‘nurturing and illustrating IV technique’ mode, we now are
- more focussed on the actual cannulation, and therefore more likely to succeed
- teaching a junior colleague, by demonstrating expert technique
- encouraging our junior colleague to approach us in future, thus ensuring safer practice
- creating a ‘micro-silence’ mindfulness moment for ourselves, as we shut out the world to focus on getting the IV in successfully
How do we make the latter choice more likely?
By practising mindfulness. By becoming aware of our own reactions, and deciding to react in another way. By taking back the reins.
Looking at it like this, why would anyone want to choose the irritability mode as our response to the request from our junior medical colleague?
But we still see colleagues, and maybe ourselves, respond to stress through the irritability mode, perhaps because they are not even aware that they are making a choice between two options, or even that there is another choice available to them.
The two frames
In other words, in most situations there are two ways to “frame” the situation, an emotionally reactive frame, and a mindful frame. The impact on those around us depends on which frame we choose to perceive the situation through, and also which frame we choose to express our reactions through.
The costs of reacting to situations in the ED through the wrong frame include:
- eroded team morale
- damage to interprofessional relationships
- staff leaving
- ED reputation damage
- negative trainee feedback
- increased clinical errors
- negative patient feedback
The overlap between mindfulness and emotional intelligence should by now be clearly evident. Current teaching about ‘ideal leadership behaviours’ draw on concepts from both domains.
Choosing the right frame – for beekeeping!
Frames are also crucial in beekeeping, carefully precise in their measurements and spacing within the hive. This discovery of ideal hive design came about as the result of much observation about what works best for the bees, and harvesting the honey without damage to the hive structure. The inventor of the modern beehive was Rev Lorenzo Langstroth, who in 1851 established an optimal hive and frame design that endures to this day.


Image: Photo taken by the author, of family members undertaking a hive check in 2020.
So, as it is with bees, it is also with our human interactions in the ED. The results we get, and the degree of collateral damage, are all related to the ‘frames’ we choose.
Thank you for reading this, and take care of yourself
A/Prof Andrew Dean FACEM
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
COVID stillness
On immunity
A systematic review1 of the literature suggests that mindfulness has positive beneficial effects on immunity, looking at various indicators of immunity including antibody formation to vaccination, activity of lymphocytes and white cell numbers in the acute phase reaction to infection.
The degree of positive effect in most studies was moderate, and would be influenced by co-morbidities and the overall health status of the person being studied. What does this tell us in a time of COVID-19?
Vaccination, with the two doses and the booster, remains our most significant protection. Other evidence-based immune-modulators in the time of COVID-19 include adequate sleep, Vitamin D, Zinc, and Vitamin C.
Interestingly, in the systematic review there were no studies showing a negative or detrimental immune system effect from mindfulness meditation, when it was compared in randomised control studies.
The form of mindfulness used in these studies was based on a standardised 6-8 week training course developed by Dr Jon Kabat-Zinn at Harvard.
COVID implications
Doing whatever we can to support our immune system, in the face of the COVID-19 Omicron variant, makes good sense. This is intuitively logical, but studies and objective supporting data are lagging behind, as is to be expected with the short history of this pandemic.
We do require further studies to ascertain the direct benefits of mindfulness with COVID-19, either within the acute illness, or with the inflammatory processes seen in the post-acute phase, and in some patients in an even longer timeframe known as “long COVID”. We just don’t have enough longitudinal data specific to COVID-19 and mindfulness, at this time, so any advice must be generic, and extrapolated cautiously from the specific immune benefits described in the article below1.
In the trenches
There are examples of how “breaks” and “time outs” are used for staff in Emergency Departments. The ED in the Landspitali Hospital in Reykjavik, Iceland, has a room for staff to quietly retreat to for mindfulness breaks during their shifts.
At the shipyard in Ketchikan, Alaska, all staff are required to undertake 15 minutes of meditation followed by stretching exercise before starting work on the ships.
The WRAP-EM team have introduced staff trollies of snacks and healthy food to help combat sagging energy levels at the Gold Coast Hospital ED.
Applying these ideas needs to be customized to the location, people and culture of any specific ED, and there are useful “how to guides”, mentioned in the book below which is aimed at the teachers of mindfulness in clinical environments2.
Setting the tone
For leaders, a crisis like COVID-19 provides opportunities to “show the way”, to be a role model, to support and nurture their team during the current times when exhaustion and stress are so prevalent.
Having our own mindfulness practice helps with managing any conflict in the workplace, as well as the challenging interdepartmental conversations that are more likely at present, due to stress at each level of hospitals during COVID-19.
The individual immune system benefits of mindfulness in relation to COVID-19 are likely but not yet proven.
Recharging the battery
Carrying stress forward from one day to the next is recognized as a factor in staff burn-out. Front-line clinicians need to cultivate activities that refresh and rebalance us, before we return to another shift.
Important in this process are physical exercise, diet, sleep, and the overall way that we think, and process emotions, particularly negative emotions. Mindfulness has its role in this domain.
Mindfulness exercise
(this one has been used with hospital staff working in a high-stress clinical area)
Duration: 5-10 minutes
Level of Difficulty: Easy
Special Equipment: Nil
- Turn off pagers or phones if you safely can
- Find a place to sit
- Close your eyes during this exercise, but only if you feel comfortable doing so
- Just study your breathing, regardless of its pattern
- To start, we are all probably “spinning fast”
- Just let that take care of itself
- Study your breathing now, flowing in, and flowing out
- It can be fast or slow, jerky or smooth, depending on the mental state you were in when you came into this room
- What it is does not matter, as this is the starting point which we will soon leave
- Just watch the breaths, as they go in, and go out
- (do this for 2 minutes if you can)
- Your breathing will slow, naturally as you observe it
- Now, move on and study your muscles as they support you
- Observe where any muscular pain or tension is
- Just observe this, and slowly scan from your toes to your head
- (do this for 2 minutes or so)
- Now as you breathe, imagine letting all the stress go out from your muscles, in your breath, away, letting it really go
- Repeat this for a few minutes
- (do this for 2 minutes or so)
- In your own time, just return slowly to the world of clinical care
- Know that you can efficiently repeat this process of balancing any time you want, and that it will become faster and faster as you practice
- Slowly stretch, and return to the room
- Thankyou for your valuable time
And to close..
These are indeed unknown times, as COVID-19 fills our radar.
Find your own stillness, if you can, each day, amidst the noise and haste.
And don’t forget to practice J
Thank you for reading this, and take care of yourself.
A/Prof Andrew Dean FACEM
References
- Black DS, Slavich GM. Mindfulness meditation and the immune system: a systematic review of randomized controlled trials. Ann N Y Acad Sci. 2016 June; 1373(1): 13–24. doi:10.1111/nyas.12998.
- Wolf C, Serpa LG. A Clinician’s Guide to Teaching Mindfulness. New Harbinger Publications. 2015. ePub ISBN 9781626251410
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
Mindfulness, then and now
A short history of mindfulness
Mindfulness and meditation crept slowly into Western countries from the early 20th Century; meditation has always been a ‘thing’ in Eastern philosophy and spirituality, and its integration in those cultures as an element of inner growth is unquestioned. We are probably familiar with the concepts of Zen, Samurai, Buddhism, yoga, tai chi and Hinduism, but perhaps less familiar with the deep roots of contemplative practice that weave through the Islamic, Christian and other great spiritual traditions.
In the 1960s and onwards, mindfulness and meditation were introduced into the West, in a significant way. The Beatles were perhaps the highest profile role-models, helping to publicise Transcendental Meditation and Eastern religion in general, to a Western mainstream, mainly young audience hungry for an alternative to the conservative status quo.
The use of illicit drugs expanded rapidly, and the drug-induced transcendental experiences from other psychoactive agents were documented by proponents such as Timothy Leary, and Carlos Castaneda, among others.
However, the psychedelics like LSD, and the plant-derived hallucinogens like psilocybin and ayahuasca, remain largely peripheral within the mindfulness movement. Mainstream meditation and mindfulness practices as taught in Western contemplative neuropsychology and clinical psychotherapy do not for the most part incorporate the use of hallucinogens. Clinical psychiatry researchers however are examining the potential therapeutic role of low doses of some of these agents in managing patients with depression and PTSD5.
In the West, two leading proponents in the development of what we understand as mindfulness were Thich Nhat Hanh1, a Zen Buddhist master, and Dr Jon Kabat-Zinn2, Emeritus Professor of Medicine at the University of Massachusetts Medical School. Kabat-Zinn has published widely and his Mindfulness-based Stress Reduction (MBSR) courses are taught across the world4. MBSR features in the curricula of many medical schools. The applications of mindfulness range from helping children with behavioural difficulties in primary schools3, to reducing PTSD and improving battlefield decisions in combat troops.
What Jon Kabat-Zinn clearly recognised, as he developed his ideas and the MBSR programme4, is that in order for concepts of mindfulness or meditation to gain traction in the Western context it was crucial that people see the relevance or value of these practices for themselves. So, in a way, we could say that the language of Buddhism was replaced with the language of neuroscience, and the idea of retreats to Thailand swapped for the findings on fMRI brain scans, during meditation. Mindfulness in this way became more approachable for the Western mind.
So here we are, after the first 50 years of the newest version of mindfulness, in a world where stress is extremely prevalent. Emergency Medicine as a microscosm of that world reflects that stress, as health care grapples with COVID-19, as well as the ongoing resourcing and staffing limitations.
How do we bring mindfulness into the day-to-day situations we are all familiar with?
“…our power for influencing the course of affairs lies not in our past, nor our future, but in the present moment.”
Transforming each moment of now
Surely this mindfulness is just an idea – which sounds nice in theory – while we are flat out in our hospital trying to keep working, despite having frontline staff in isolation due to COVID, closures of crucial services in the hospital, and an Emergency Department that never empties?
So many elements in this pandemic are indeed beyond our control. Imperfect political decisions, shortages of PPE and diagnostic resources, the bewildering behaviour of those in our population who resist vaccination – the potential for us to be overwhelmed by this is real, and some are overwhelmed by it all.
And yet, a leader must stand apart from the fray, and simply lead. Anyone who would remain effective through a crisis knows this simple fact: that our power for influencing the course of affairs lies not in our past, nor our future, but in the present moment. And, yes, we are all asked to be leaders, in our own role.
Thich Nhat Hanh encapsulates how we can bring mindfulness into the midst of chaos, by stripping the complexities down to the ‘now’ moment that we find ourself in.
“Remember that there is only one important time and that is now. The present moment is the only time over which we have dominion. The most important person is always the person you are with, who is right before you, for who knows if you will have dealings with any other person in the future? The most important pursuit is making the person standing at your side happy, for that alone is the pursuit of life.”
Thich Nhat Hanh, 1975
from The Miracle of Mindfulness: An Introduction to the Practice of Meditation1
In our context in the ED, our series of moments might line up something like this:
- take a history mindfully from a patient,
- cannulate the next patient with mindful focus,
- guide a safe procedural sedation with mindful oversight of all the staff and the patient
- discuss bed problems with the overburdened patient flow coordinator in a mindful and supportive way
- take a short coffee break and make it a mindful regrouping time
- finish our documentation with full focus
Each moment with another person can be viewed as a transaction which, when conducted in a mindful manner, becomes a net positive contribution to the welfare of every person you are interacting with. You will have the satisfaction of knowing that you gave that moment your complete mindful attention, which most certainly will be noticed by each person you met.
It certainly is food for thought, and given the intrinsic and extrinsic stressors that are endemic (?pandemic) to our clinical ED practice here at the start of 2022, surely we should be seriously looking at how a mindfulness practice can help smoothe the journey ?!
Thankyou for reading this, and take care of yourself.
A/Prof Andrew Dean FACEM
References:
- Hanh, T,N. (1996). The Miracle of Mindfulness: An Introduction to the Practice of Meditation. Boston, MA: Beacon Press; 1975.
- Kabat-Zinn, J. (2005). Wherever you go, there you are: Mindfulness Meditation in Everyday Life. Hachette Books
- Burnett, R., and Cullen, C. (2010). The Mindfulness in Schools Project. http://www.mindfulnessinschools.org.[Google Scholar]
- Kabat-Zinn, J. (2011). Some reflections on the origins of MBSR, skillful means, and the trouble with maps, Contemporary Buddhism, 12:1, 281-306, DOI: 10.1080/14639947.2011.564844
- Fuentes, J., Fonseca, F., Elices, M., Farre, M., Torrens, M. Therapeutic use of LSD in Psychiatry: A Systematic Review of Randomised-Controlled Clinical Trials. Frontiers in Psychiatry. 2019; 10: 943
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
Mindfulness 102
Summarising – yet again
At its most basic level, mindfulness is a retraining of our default emotional responses to stress and ‘triggers’. By constant and deliberate application of another set of responses, that is, the calm and mindful responses, we grow to realise that the situations outside us are separate from our emotional and physical reactions to them. By progressively detaching ourselves from ‘doing anger’ and ‘doing irritable’, external stressor situations lose their sting. The situations themselves become less painful.
And, because we are coming from a calmer response, we also cause less collateral emotional damage to others around us, and thereby help them in their journeys. We teach in every moment, by the way we behave and react.
“We teach in every moment, by the way we behave and react”
“That’s all very theoretical”, you could say. Let’s break it down into three broad areas.
The three-pronged approach to mindfulness
Mindfulness practice can be viewed as comprising three main domains. This could be described as a “three-pronged” approach.
- A cognitive framework of ongoing psychological or spiritual growth
- A moment-to-moment retraining of our default responses to stresses, both ‘outer’ and ‘inner’
- A daily dedication to longer practice sessions by which we accelerate our understanding
Mindfulness requires work. It also requires a readiness in us to acknowledge that our previous patterns of reaction are causing us hurt, and perhaps also to others around us. Without a willingness to start what is for some quite profound inner change, the metaphorical “train” does not really “leave the station”.
Choosing our cognitive framework
This will be an individual choice. The range of cognitive frameworks for mindfulness and related explorations can be likened to taking an ECG on a patient. Each ECG lead records the same electrical phenomenon, but from a slightly different perspective, and the resulting recordings are slightly different. In mindfulness, we each choose our starting perspective – based on our preferences and past experiences.
The “hard science” model
Our minds may be more comfortable with a “hard science” approach to mindfulness, for example, an approach which looks at objective and measurable indicators of stress reduction, with evidence-based scientific studies as a backdrop. Such studies provide discussion of EEG evidence of increased brain wave coherence as we incorporate mindfulness into our day. Other papers show objective anatomical changes in the brain structure of meditators when examined in an fMRI scanner, compared to a control group of non-meditators.
The methodology of mindfulness practice in the “scientific” paradigm would be completely “unfluffy ” and free of any “weird stuff”, focussing instead on the methods of breathing techniques for relaxation and body scanning exercises, and watching for observable improvements in stress and mood, or reduced conflict in our relationships.
This approach is probably the “best fit” initially for most of us in emergency medicine, who come from a clinical and scientific starting point. Jon Kabat-Zinn had this in mind when creating his books and training courses in Mindfulness Based Stress Reduction (MBSR). Without a clear compatibility with the way many people conceive of our mind and consciousness, the uptake of mindfulness in the West would have been more limited. Instead, his model of mindfulness has expanded rapidly across Western medical schools, and in many other community groups, including schools. Kabat-Zinn continues to have a prominent influence, and is one of many well known “change leaders” in the development of mindfulness practice in our context.
The “spiritual growth” model
It’s fair to say that many people working in the emergency department would not call themselves spiritual, and the label would sit uncomfortably for those. Hence the value of a “hard science” model for mindfulness for emergency clinicians, which makes these concepts more approachable. I know that such stereotyping is not an accurate portrayal of all emergency clinicians, but the general idea may remain useful as a starting point.
But there is also no denying that the science of mindfulness and meditation developed in parallel around the globe, beginning some 2000 years ago, as an element of the world’s great religious and philosophical traditions. Individual experiences of the “something greater than me”, or a sense of the “profound”, have probably always intrigued humans, to varying degrees.
This sense of curiosity about the ‘profound’ motivates some to study philosophies like Buddhism, for one example. Buddhism perhaps provides the neatest “fit” with modern Western mindfulness, and most of its concepts are paraphrased from established Buddhist meditation techniques. Dr Jon Kabat-Zinn himself was a Buddhist teacher, and from this he developed a “Western” mindfulness model2.
To learn about Buddhism, the three-pronged approach I described above would consist of, firstly, the cognitive elements in the ancient texts and sutras, and then the other two “prongs” would comprise “right daily living” practice, and then several daily longer meditation periods1. A large element of the Buddhist “curriculum” is based on structured meditation training and experience. The meditation, or mindfulness, components help to integrate the theoretical framework with subjective experience that, interestingly, builds a common sequence of learning and experience that is fairly similar between different practitioners2. The Buddhist sutras recognise this commonality in mindfulness practice, and describe maps of the shared learning stages3.
Dr Daniel M Ingram is an American emergency physician and Buddhist, and author of “Mastering the Core Teachings of the Buddha: An Unusually Hardcore Dharma Book”3
This mindfulness stuff is everywhere, it seems!
Buddhism is but one example of various spiritual or philosophical self-development paths, that use structures incorporating mindfulness elements into the “training course”.
Yoga and mindfulness
Another well-known example is yoga, which certainly involves the asanas (body positions), and progressive musculoskeletal training. This sounds a bit like physiotherapy, if we just describe yoga using the “hard science” model, but yoga also incorporates a deliberate slowness in the movements and asana transitions, that naturally brings the practitioner’s mind into a relaxed or meditative state. It is hardly surprising that we often incorporate yoga sessions into our ACEM Annual Scientific Meetings, as a counter-balance to the fast-paced life of emergency medicine!
A further component of yoga, or similar movement-based martial arts like tai-chi, is that we stop talking during the practice, which allows for the experience of mindfulness to develop naturally. In itself, silence alone helps to provide a space to help us recalibrate our levels of nervous tension.
“In itself, silence alone helps to provide a space to help us recalibrate …”
Meditation and spirituality overlap in many ways. Further examples include people who use nature as a rebalancing environment. When a person goes into a natural or wilderness environment, and spends some time sitting in mindfulness or meditation practice, the experience seems to be heightened or reinforced by just being in that place. The pursuits of fishing, or kayaking, or bushwalking quietly, create an automatic form of mindfulness, or increased mental coherence.
So, what is the common thread in all the above approaches to mindfulness? Firstly, the introduction of silence, or relatively few words. Additionally, slowly going through a repetitive activity. One foot in front of the other, in a slow walking rhythm, or one cast of the fishing rod after the other, and a lot of standing still perhaps waiting for the fish to bite. Mindful biting, of course.
The physical environment itself also has a measurable effect on our mental state, which is intuitive but not completely understood, and which is increasingly being utilised in the design of public spaces, to enhance community wellbeing. ED architectural design could utilise such principles to a much greater extent than we currently do.
For those already interested in exploration of their own spirituality, whatever they conceive this to be, there are many approaches which incorporate mindfulness. The language might be different. Those coming through a religious or faith-based entry point into mindfulness might call the process prayer.
So, there are many options. Wherever we start from, the likelihood is that we will change our understanding significantly along the way, as we experience the definite benefits.
One common element that develops at some point is trust. By practising the three-pronged elements described above (remember that they are: cognitive framework, moment-to-moment mindfulness, and daily mindfulness practice sessions), our own experience of benefits will start. There will likely be different experiences and rates of change for different individuals, but it will start.
And then, to our surprise, we will discover that we can change our patterns. This, in turn, builds a nascent sense of trust that we can effect such changes, and increase our enjoyment of this thing called life.
If we are coming through a spiritual paradigm to mindfulness, the word we might use instead of trust might be faith. Regardless of terminology, the overall process is similar, no matter how we try and select words to describe what is happening.
And in closing …
So, are the two models described above really so separate after all? The distinctions actually become blurry, just as they do in modern cosmology or quantum physics.
In the next instalment, we will look at some “in the moment” breathing techniques that can help us mentally and emotionally “change tracks” right in the midst of stress, both in the ED, and also in life outside the hospital walls.
Thankyou for reading this, and take care of yourself.
A/Prof Andrew Dean FACEM
References:
- Hanh, T,N. (2nd edition 1996). The Miracle of Mindfulness: An Introduction to the Practice of Meditation. Boston, MA: Beacon Press; 1975.
- Kabat-Zinn, J. (2005). Wherever you go, there you are: Mindfulness Meditation in Everyday Life. Hachette Books
- Ingram, D.M. (2018). Mastering the Core Teachings of the Buddha: An Unusually Hardcore Dharma Book. Aeon Books Ltd. ISBN-13: 978-1-91159-710-0. Also see website integrateddaniel.info/book Accessed 28th January, 2022
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
Practice arenas
Reframing 102
“the spaces we move through each day are a series of practice arenas; opportunities to learn just how powerful we can be, if we get this stuff right..
The spaces we move through each day are a series of practice arenas; opportunities to learn just how powerful we can be, if we get this stuff right. Examples include the conversation with a consultant, the inclusion of an ED patient in the ward round, a meeting with a “challenging” relative, and all of our interactions with medical colleagues, nurses and clerical staff. Was each interaction with each person our best work? Did we look after them?
It is easy to stay in our old patterns, seeing ourselves as weighed down in conflicts and difficult situations, or we can lift above the noise, and increase our efficacy as healers. Yes, we put on our own oxygen mask first; starting to mindfully approach every interaction we have, every thought, and then watching our culture-nurturing role become so much simpler within the ED, or wherever we might find ourselves. We take up that proverbial polishing cloth, like a lighthouse keeper; and just keep cleaning our lens, and watching the carbon fall away from the glass.
Be like the lighthouse keeper; just keep cleaning the lens, and watch the carbon fall away from the glass.
Rescue strategies
Patterns can change.
Mindfulness is but one of the tools that make a career in emergency clinical care just that much easier; if we are constantly giving out quality and compassionate care to our co-workers and patients – which we should be – the “energy recharging” process needs to be very conscious, or we run the real risk of becoming depleted ourselves. We cannot be a support for others until we are solid in ourselves.
“We cannot be a support for others until we are solid in ourselves”
Reflecting on kidnapping, the Stockholm syndrome, and mindfulness…
Once we realise how much these unhelpful thought patterns weigh us down – patterns like hate, anger, judgement, resentment or irritation – and how those reactions create tiredness and perhaps physical ailments in us, the attraction fades very quickly. Or it should.
Why then are we attracted to reacting repeatedly in negative patterns? Maybe the opposite question is easier to grapple with – why is instituting changes in our default emotional reaction patterns so uncomfortable?
In the “kidnapping literature” (if there is such a thing) they have a term called the “Stockholm syndrome”. One definition is:
“Stockholm syndrome, a psychological response wherein a captive begins to identify closely with his or her captors, as well as with their agenda and demands.”4
“But exactly how does kidnapping tie in with mindfulness?”
Our patterns of established reactions do seem to resist change, even when our health can only benefit from such changes. We perhaps identify too closely with the reaction patterns – as if they were like the “captors” in the Stockholm syndrome – and we agree to the agenda and demands of those “captors”, even when it hurts us. We may hold on to those patterns as a perceived survival mechanism, like the person held captive.
Considering these patterns may have developed over several decades, becoming “hard wired” into us, it does take application to reverse those patterns. But we are no strangers to hard work as emergency and critical care professionals, and we do have the capacity to concentrate. The change required is possible.
And minute by minute, hour by hour, we can monitor our thoughts and reactions, and simply ask: “Is this a mindful response? Is this my best work?”
In other words, the practising of mindfulness is now, and tomorrow, and all the time.
Breathing 102
So, let’s look at breathing, again.
Breathing awareness is not something that we have in full focus all the time, and we do need to “tune it out” when actively involved in conversations, or when making clinical decisions.
However, when we are confronted with a deteriorating patient, there are still moments of recalibration, when we can take a few mindful breaths. I remembered to do this today, when faced with being team leader in an unfamiliar resuscitation scenario. It felt scrambled at the start, so I took a few seconds for slow and steady deliberate and mindful breaths. This helped me to quickly “centre”, and I was able to be more effective in my diagnostic reasoning and leadership, and everything seemed to flow better.
So, what about this breathing?
Breathing exercises can be approached using the three-pronged approach to mindfulness, discussed in the previous blog (Mindfulness and the ED doctor #16)5.
Breathing strategies can be applied “on the run” as a moment of anxiety, conflict or any other threat to you sense of calm is detected.
They are applied differently in designated “practice periods” when you set aside a time, perhaps as little as 5 minutes, but increasing to 10 minutes, or even a 20-minute session each day, as you feel comfortable.
Breathing on the run
At the very moment that you sense stress in yourself, remember something very simple.
Make this into a discipline, and each time you remember, you will reinforce your capability to return to a sense of calm, regardless of the external situation. Yes, of course we all forget initially, but progressively we collectively will remember.
At each stress moment, structure your next few breaths to be slower and deeper, using a counting technique such as “one… two… three… four” spaced about a second apart, as you breathe in.
As your lungs are filled, briefly pause, then as you breathe out count back “four… three… two… one”, again spacing the numbers over about 4 seconds.
Repeat this, making it your absolute focus, for a few more breaths. You may have to curtail the number of breaths if the external situation is urgent, but even one structured breath will enable you to change tracks, as it were, to a more mindful place from which to create your response to the situation.
Taking control of your breathing reminds your mind that you are the boss, the executive in control. The anatomical correlation is that you are deciding during your breathing exercise to give the prefrontal cortex (our emotional regulation centre) more prominence than the amygdaloid nucleus (our “fight and flight” reflex centre).
As your physiological reaction to the external stress starts to become calmer, you might use some affirmations like “I’ve got this”, or whatever resonates with you. Affirmations reinforce the change you are creating in your default reaction, and are another one of the many mindfulness strategies available.
Breathing for longer practice periods
Do you remember way back in the early articles, how I mentioned the transition zone techniques that we can utilise either singly, or all at once, to train our mind in the early difficult entry from “daily life” into “stillness”?
We will look at each of these in more detail, but firstly breathing. As you sit for a more extended period, the 4 seconds/4 seconds cycle can be the starting point, and as this feels comfortable, extend the times to a 4 seconds inspiration / 8 seconds expiration pattern, and even slower as you can. You may need to adjust the depth of breaths and don’t become breathless in your efforts; simply take a few recovery breaths and then try the progressive slowing again.
By watching and regulating your breathing, the “stress” thoughts and their associated emotional reactions are effectively starved of oxygen. In their place, stillness starts.
In deep relaxation, you may find that you actually have pauses in breathing, or that your respiratory rate decreases significantly for a time, as your mind becomes really still.
Try it for yourself.
Thankyou for reading this, and take care of yourself.
A/Prof Andrew Dean FACEM
References:
- Hanh, T,N. (2nd edition 1996). The Miracle of Mindfulness: An Introduction to the Practice of Meditation. Boston, MA: Beacon Press; 1975.
- Kabat-Zinn, J. (2005). Wherever you go, there you are: Mindfulness Meditation in Everyday Life. Hachette Books
- Ingram, D.M. (2018). Mastering the Core Teachings of the Buddha: An Unusually Hardcore Dharma Book. Aeon Books Ltd. ISBN-13: 978-1-91159-710-0. Also see website integrateddaniel.info/book Accessed 28th January, 2022
- Stockholm syndrome – definition, examples and facts. https://www.britannica.com/science/Stockholm-syndrome
Accessed 14th Feb 2022
- Dean, A. Mindfulness and the ED doctor – Article 16. Jan 2022. Life in the Fast Lane. litfl.com
Waiver: These articles represent my own views and approach to mindfulness, and do not purport to be the official view of ACEM. They are not intended to replace appropriate medical or mental health care, provided by professionals in these domains.
Expansion
All the time, but especially now in our emergency departments, we need teams who are self-regulating and emotionally intelligent. Another way of describing this is to state that the people in the ED clinical team are, ideally, practitioners of mindfulness in some way, even if they do not necessarily use such wording themselves.
It is lucky indeed for an ED if a few individual nurses and doctors are consciously working on mindfulness practice – by doing yoga, for example, or by meditating, or by reading books that they find inspiring. Individual mindfulness is one thing, but it is much more effective if a team of clinical staff are consciously and deliberately using mindfulness principles every day, in the way that they deliver emergency clinical care.
A mindful ED clinical team does not happen by chance, but by design.
What does this mean in the real world?
Using team “time outs” before we sedate someone in the ED is an automatic habit for me now, but we all know ED clinicians who do not use time-outs.
Operating theatres have similar challenges with their clinicians, with attitudes leading to non-compliance with time-outs. Embedding permanent change in the safety culture is an ongoing challenge for all critical care areas.
So, as I called a “time out” the other day, we realised that we did not have additional IV fluid attached in case the patient dropped their blood pressure during sedation. The situation was fixed immediately, but the pre-sedation checklist was crucial in detecting this potential problem before we started the procedure.
What was mindful about this?
The staff all felt calm and listened to. The patient was included in our discussion of what we were about to do, and was advised what drugs we would be using, as an element of obtaining their informed consent. There was a deliberate calm in the room. The IV fluid error was detected as went through the checklist.
“When done well, these time-outs reflect a patient-centred safety culture and develop an environment of trust in staff who are empowered to report patient safety events without fear of reprisal, while acknowledging that humans are fallible and make mistakes.”
“During the time-out, the team comes together and develops a shared mental model of what the procedure will be like, increasing the chances that all members will have the situational awareness needed to prevent harm. It also establishes the leadership of the team and empowers all members to work on behalf of the patient. Administration of drugs, control of glycaemia, allergies, and other factors that can affect an operation’s outcome are discussed in these briefings.” 2
So, what if the opposite situation had occurred?
Into the procedure room might come an aggressive and hasty senior doctor, speaking to no one in particular, just demanding that the procedure be “started”. Team members are now grappling with a sense of stress, concerned about receiving further negative comments from the senior doctor.
This might well reduce the team’s focus on the checking, and the belligerent senior clinician might then impatiently interrupt the checklist process, or try and “skip it” altogether. The lack of connected IV fluid may not have been detected, and during this hypothetical situation the BP could have then fallen to a dangerously low level.
Atul Gawande describes the links between team mindfulness and safety in his several books about safety culture in the operating room environment1, and he provides concepts that we can also apply in the ED environment.
The contrast between nurturing staff (mindful team approach, inviting input into the time out, etc.), and psychologically undermining staff, is enormous, and the implications extend beyond the safety example described above. Staff resign from full-time positions in emergency departments, because of even one such unpleasant situation, where senior clinicians did not relate mindfully and caringly to the other members of their ED Team.
This is familiar to us all – sadly – and should act as an encouragement for us to apply the mindfulness principles in our EDs and hospitals.
But it all starts at an individual level. One person decides to change something in their own life, and that begins a ripple effect.
So here is another practice session that may be useful as a concept for your own mindfulness practice.
Mindfulness practice session
Find a quiet place; this will take 10 minutes.
Phones off. Get comfortable in your chair.
Start breathing down from “waking” to “mindfulness” level, focussing on breathing, becoming really aware of the smooth timing and rhythm of the in-breaths, and the out-breaths.
Feel muscles loosen.
As you start to hit that feeling of calm, imagine it to be like a stop point on a “free dive”. Adjust to this level of calm, and don’t worry if distracting thoughts come. Just catch yourself, and re-focus on your breathing cycles.
And let go, and metaphorically dive down the rope again.
Now imagine that you are reaching a level of calmness that is one hundred times calmer than the first calm level you reached.
Recalibrate at this new level; you are becoming very still, very quiet.
Move on down the rope again.
Now imagine that you are reaching a level one thousand times more peaceful than the preceding stage.
How slow your breathing is now.
The mental “noise” is fading away.
Some distractions come up occasionally, but they have lost traction even as they arrive, and they fade away.
Hold this level for a while, then slowly set the intention of returning to the 3D physical world.
Slowly wake up, stretch your limbs, and return to “daily life”.
The scattering
This will be my final article in this mindfulness series. I am very humbled and grateful for the positive feedback that the articles have generated. Also, I am incredibly appreciative to the editor of this publication, for the invitation to write the series of articles.
These articles have been presented in the hope that the ideas contained may be useful for you.
Mindfulness ripples outwards, as we incorporate it into our daily thinking, and our daily programme. It changes everything.
I will now be focussing on a mindfulness project of another sort. I have joined the creative and editorial team, for an upcoming film documentary about a spiritual text called A Course in Miracles.
…but that is a story for another day.
And in closing
Our quote today comes from the French philosopher and theologian, Pierre Teilhard de Chardin.
“Driven by the forces of love, the fragments of the world seek each other, so that the world may come into being”
Pierre Teilhard de Chardin3
Thank you for reading this.
A/Prof Andrew Dean FACEM
References:
- Gawande, A. (first edition 2009). The Checklist Manifesto. Metropolitan Books.
- https://bulletin.facs.org/2017/06/time-outs-and-their-role-in-improving-safety-and-quality-in-surgery/ Bulletin of the American College of Surgeons. Accessed 1st April, 2022
- Teilhard de Chardin, P. (1881-1955)